To learn more about a breast change, you may need an ultrasound, an MRI, a biopsy, or other follow-up tests.

Ultrasound
An ultrasound exam uses sound waves to make a picture of breast tissue. This picture is called a sonogram. It helps radiologists to see if a lump or mass is solid or filled with fluid. A fluid-filled lump is called a cyst.
MRI
Magnetic resonance imaging, or MRI, is a technique that uses a powerful magnet and radio waves to create detailed images of breast tissue. Sometimes breast lumps or large lymph nodes are found during a clinical breast exam or breast self-exam that were not seen on a mammogram or ultrasound. In these cases, an MRI can be used to learn more about these changes.
Breast Biopsy
The breast surgery clinic under Dr. Khare offers a complete package to do a biopsy of a suspected breast lesion.
A biopsy involves removing tissue or fluid from the breast so that it can be examined under a microscope and further examined.
You may have heard a lot of different terms to describe your cancer if you’ve been diagnosed with it. During a breast biopsy, doctors learn a lot about the type of cancer you have. You may also need more tests to get more details, such as the stage of the cancer or how fast it’s growing.
Common types of breast biopsies:
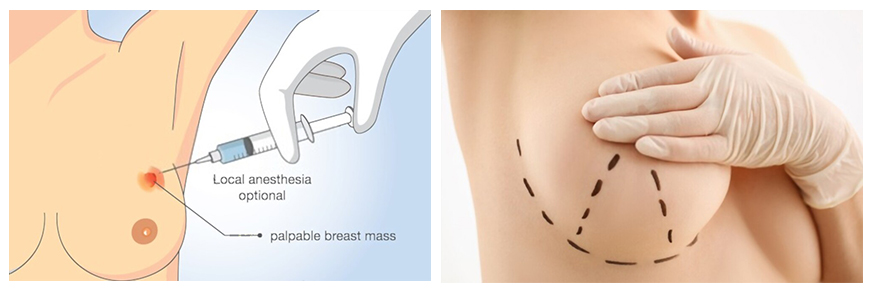
- Fine-needle aspiration biopsy
FNA is a method of obtaining fluid or tissue samples from cysts and solid masses using a thin needle inserted into the skin. FNA, the doctor uses a very thin, hollow needle attached to a syringe to withdraw (aspirate) a small amount of breast tissue or fluid from a suspicious area.
A FNA is often performed if the suspicious area is likely to be a fluid-filled sac. By removing fluid, the FNA can often help relieve pain from the cyst. The doctor can also use FNA if they are unsure if an area seen on an imaging test is a cyst or a solid mass.
- Core biopsy
A core biopsy involves passing a needle through the skin to obtain tissue samples from a lump or mass. The tissue is then examined under a microscope for any abnormalities
Core biopsy is performed with the use of local anesthetic to numb the area where the needle is inserted. A small incision (cut) is made in the skin over the lump, and a needle is inserted through the incision
- Vacuum-assisted biopsy
A vacuum-assisted biopsy uses a probe, connected to a vacuum device, to remove a small sample of breast tissue. The small cut made in the breast is much smaller than with surgical biopsy. This procedure causes very little scarring, and no stitches are needed.
- Surgical biopsy
Surgery biopsy involves removing all or part of a lump so it can be examined under a microscope for signs of disease. Sometimes a doctor will do a surgical biopsy as the first step. Other times, a doctor may do a surgical biopsy if the results of a needle biopsy do not give enough information.
When only a sample of breast tissue is removed, it’s called an incisional biopsy.
When the entire lump or suspicious area is removed, it’s called an excisional biopsy.
“Core biopsy is performed with the use of local anesthetic to numb the area where the needle is inserted. A small cut is made in the skin over the lump, and a needle is inserted through the incision.”

Hormone receptors and protein markers
About one-half of breast cancers require the female hormones to grow. Hormone dependent breast cancer cells produce proteins called hormone receptors, which can be estrogen receptors (ER), progesterone receptors (PR), or both.If hormone receptors are present within a woman’s breast cancer, it is likely to benefit from drugs that block the action of estrogen. These treatments are referred to as hormonal therapy. Hormonal therapy is usually recommended to all patients with ER-positive breast cancer, even if the lymph nodes are negative, because it generally has less toxicity than chemotherapy and lowers the chances of developing a second breast cancer in the future. In contrast, those cancers that do not contain any ER or PR do not benefit from hormone therapy.
HER2 is a protein that is present in about 20 percent of invasive breast cancers. The presence of HER2 in breast cancer identifies women who might benefit from treatments directed against the HER2 protein. Drugs that target the HER2 protein include trastuzumab (Herceptin), pertuzumab (Perjeta), ado-trastuzumab emtansine (Kadcyla), and lapatinib (Tykerb).
Extent of involvement and spread outside the breast
Once a diagnosis of breast cancer is established, the next important questions are how extensive is the cancer involvement within the breast and is there evidence of spread of the cancer outside the breast.
While breast cancer starts within the breast, few cancer cells may break off and spread outside the breast. This process of spread outside the breast is called metastasis. Metastasis can occur to lymph glands or to an organ such as the liver, lungs or bones. The metastasis may produce a mass or lump. They can also cause symptoms such as bone pain. Metastasis can be identified on a computed tomography (CT) scan, a bone scan, or a positron emission tomography (PET) scan.
The importance of the axillary lymph nodes
One of the first sites of breast cancer spread is to the lymph nodes located in the armpit (axilla). These nodes (axillary lymph nodes) can become enlarged and can sometimes be felt during a breast examination. They can also be detected on the mammogram or MRI. The presence or absence of lymph node involvement is one of the most important factors in determining the long-term outcome of the cancer and it often guides decisions about treatment .If the axillary lymph nodes contain cancer (positive nodes), there is a higher chance that cancer cells have spread elsewhere, and most of these women will need chemotherapy.
Examination of the axillary lymph nodes
The axillary lymph nodes should be examined for tumor spread. This is done first by physical exam and sometimes with ultrasound. If a suspicious lymph node is found, then a needle biopsy to obtain a tissue sample is performed. If there is cancerous involvement of the axillary lymph nodes, a surgical procedure called axillary lymph node dissection is performed at the time of the breast surgery to remove all the nodes from the axilla.
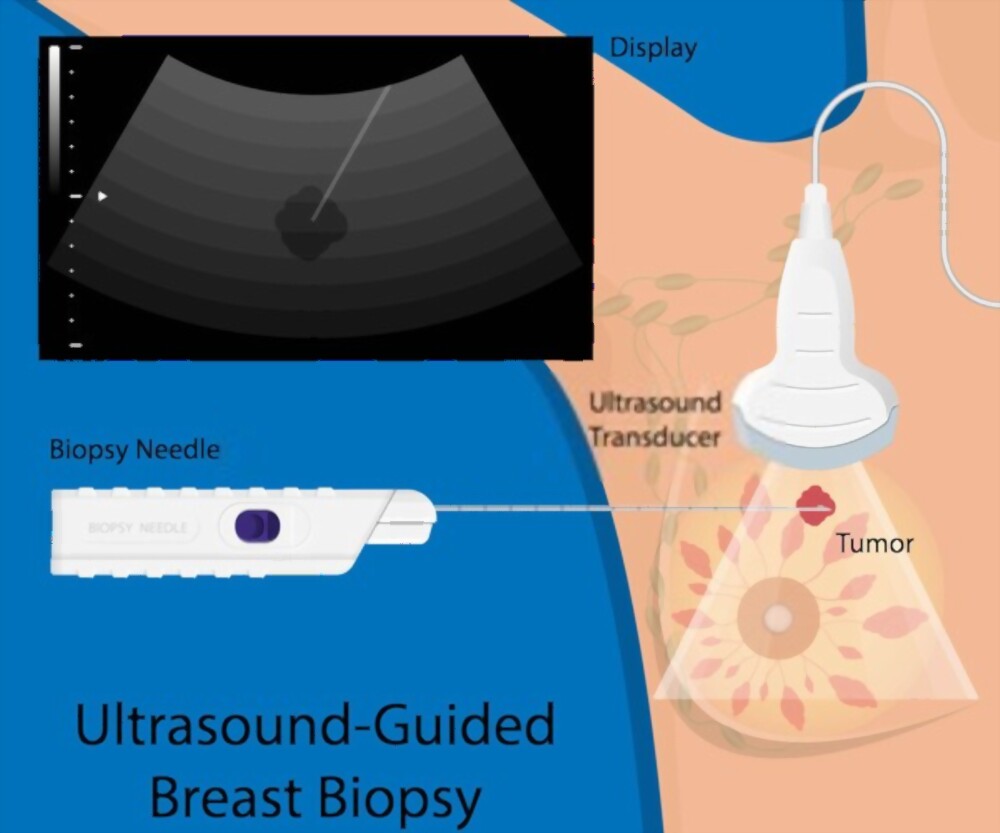
The importance of the axillary lymph nodes
One of the first sites of breast cancer spread is to the lymph nodes located in the armpit (axilla). These nodes (axillary lymph nodes) can become enlarged and can sometimes be felt during a breast examination. They can also be detected on the mammogram or MRI. The presence or absence of lymph node involvement is one of the most important factors in determining the long-term outcome of the cancer and it often guides decisions about treatment .If the axillary lymph nodes contain cancer (positive nodes), there is a higher chance that cancer cells have spread elsewhere, and most of these women will need chemotherapy.
Examination of the axillary lymph nodes
The axillary lymph nodes should be examined for tumor spread. This is done first by physical exam and sometimes with ultrasound. If a suspicious lymph node is found, then a needle biopsy to obtain a tissue sample is performed. If there is cancerous involvement of the axillary lymph nodes, a surgical procedure called axillary lymph node dissection is performed at the time of the breast surgery to remove all the nodes from the axilla.

Sentinel lymph node biopsy
In patients with early-stage breast cancer who do not have obvious involvement of the axillary lymph nodes, a surgical procedure called a sentinel lymph node biopsy is often performed. In this procedure, special tracers are used to mark the lymph nodes that the cancer is likely to spread to (also called “sentinel” nodes). These lymph nodes, which are usually under the armpit, are then removed for pathological analysis. The major benefit of the sentinel lymph node procedure is that it provides important staging information while causing fewer problems such as arm swelling (also called lymphedema) than a more extensive axillary lymph node dissection. If sentinel lymph nodes do show presence of cancer, then removal of the remaining axillary lymph nodes would be needed.

21 gene test (Oncotype DX)
A genetic test called Oncotype DX Recurrence Score (RS) can be performed on the tumor tissue to help with decision making about chemotherapy, especially for women with ER positive, HER2 negative, and lymph node-negative breast cancer. The test looks at 21 different genes in order to evaluate the genetic makeup of the tumor and provides a numerical score to help predict the chance of recurrence. The score is called the “Recurrence Score,” and it ranges from 0 to 100. In general, patients with a low recurrence score whose cancers also have other low-risk features may not need chemotherapy, whereas those with a high score benefit more from chemotherapy.

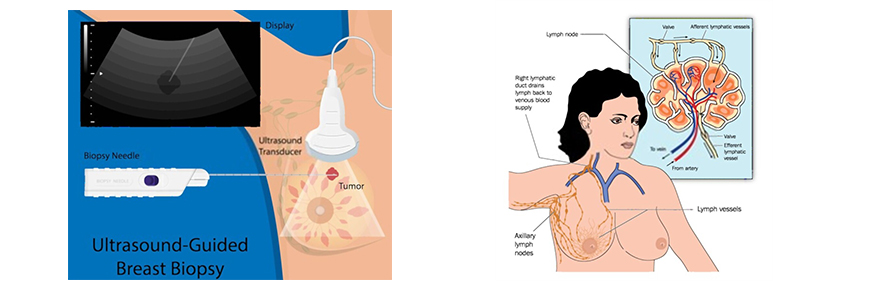
Stereotactic Breast Biopsy
During stereotactic breast biopsy, low-dose x-rays are used to locate breast abnormalities and remove a sample of tissue for examination under a microscope.
The procedure is less invasive than surgical biopsy, leaves little to no scarring, and can be extremely useful in evaluating calcium deposits and tiny masses that are not visible with ultrasound.
Tell your doctor if there’s a possibility you are pregnant. Discuss any medications you’re taking, including aspirin and herbal supplements, and whether you have any allergies — especially to anesthesia.
Doctors use breast biopsy to remove a small amount of tissue from a suspicious area for lab analysis. The doctor may perform a biopsy surgically. More commonly, a radiologist will use a less invasive procedure that involves a hollow needle and image-guidance. Image-guided needle biopsy does not remove the entire lesion. Instead, it obtains a small sample of the abnormality for further analysis.
What Our Patients Are Saying About Us


